The Cost-Effective Health Plan Solution Offered by Major National Carriers
By leveraging KelseyCare’s innovative model of coordinated care, your clients will experience the benefits of:
By leveraging KelseyCare’s innovative model of coordinated care, your clients will experience the benefits of:

Health benefits expert, Shelley Tarkington, explains how KelseyCare Health Plans offers a healthy business strategy, resulting in healthier employees and a healthier bottom line for your clients.
KelseyCare manages expenses more effectively than broad network PPO and HDHP plans resulting in 15-30% total medical cost savings. Healthcare costs are managed more effectively through our physician-led model of care that focuses on prevention and proactive disease management. Our integrated, coordinated care model is based on doctors working together to deliver high-quality care.
Brokers, connect with our team to explore case studies about total medical cost savings and uncover real business benefits.

At KelseyCare, we're proud to offer the trusted brand of Kelsey-Seybold Clinics.
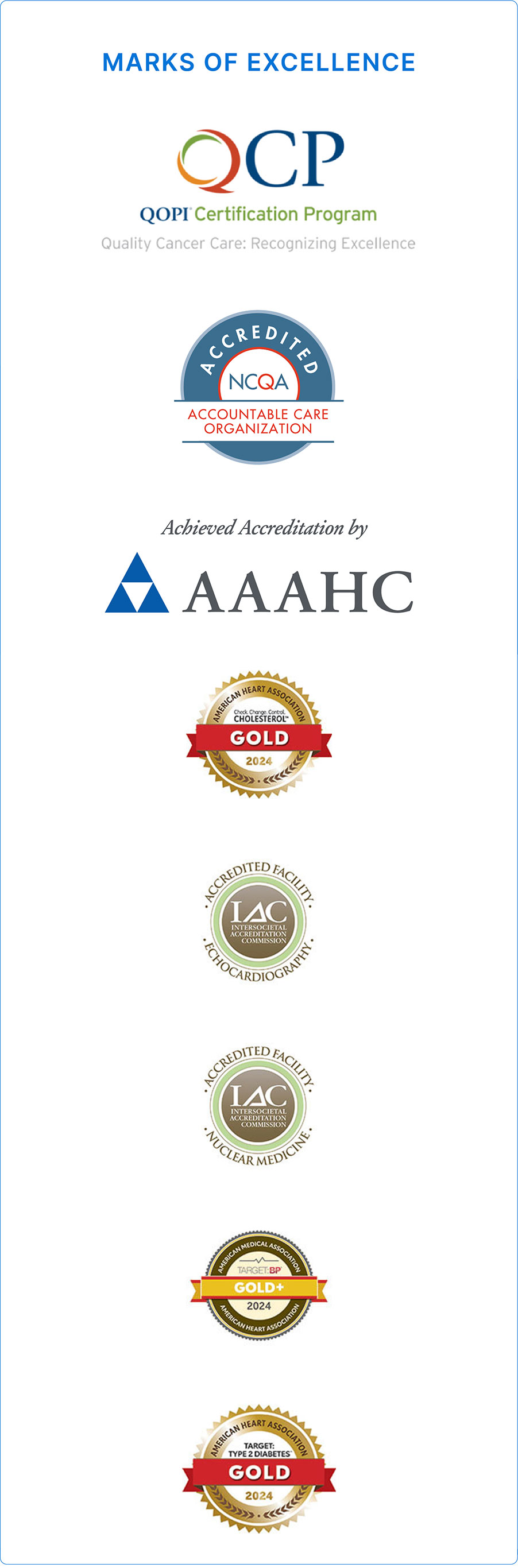
As the nation’s first NCQA accredited Accountable Care Organization (ACO), KelseyCare is fundamentally different from any other health plan with one goal in mind: improving health. This benefits everyone with higher employee health and member satisfaction, and lower total medical cost. Plus, employees will appreciate accountable, coordinated care for their entire health journey.
You and your clients can count on dedicated account support for any needs.

With 40+ locations around Greater Houston and growing, KelseyCare is a convenient option for your clients’ employees. All under one roof, KelseyCare provides coordinated, compassionate care through multispecialty care centers*, a cancer center, women’s health center, ambulatory surgery centers, and a specialized center, all with hospital affiliations that you can trust.
Convenient clinic locations close to work and home around the Greater Houston area.
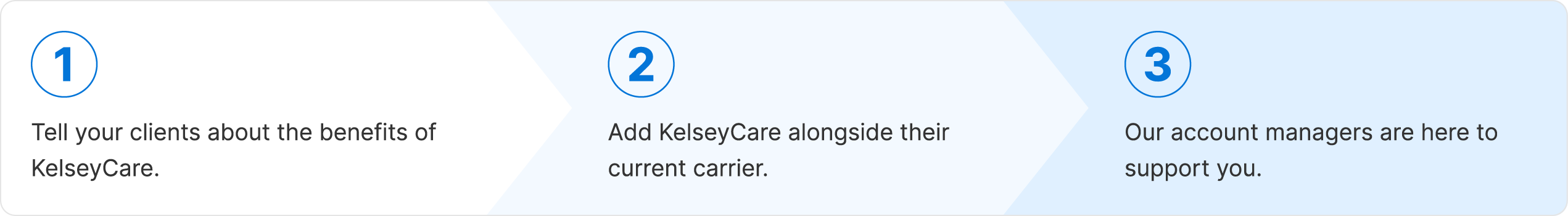
It's simple to add KelseyCare. Your clients simply add KelseyCare as a plan choice alongside existing plans. It is available as an option for Greater Houston region employees with no disruption to employees outside the service area.





