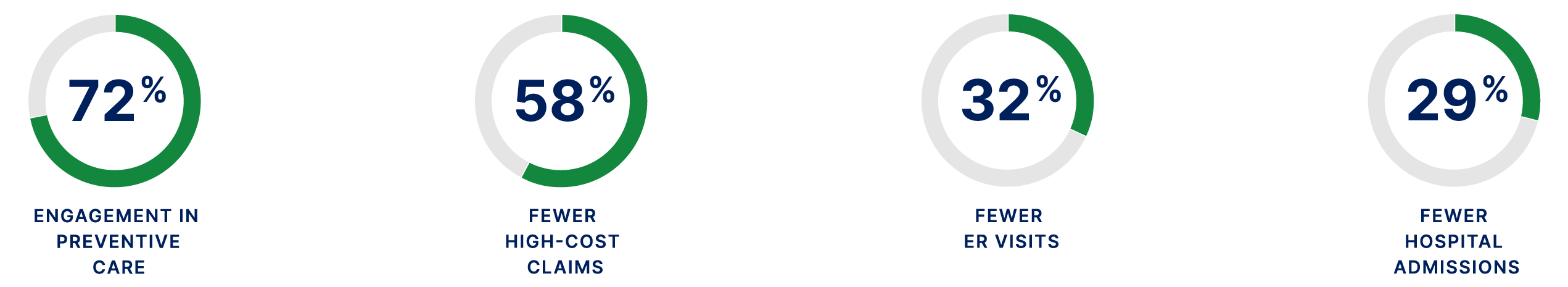
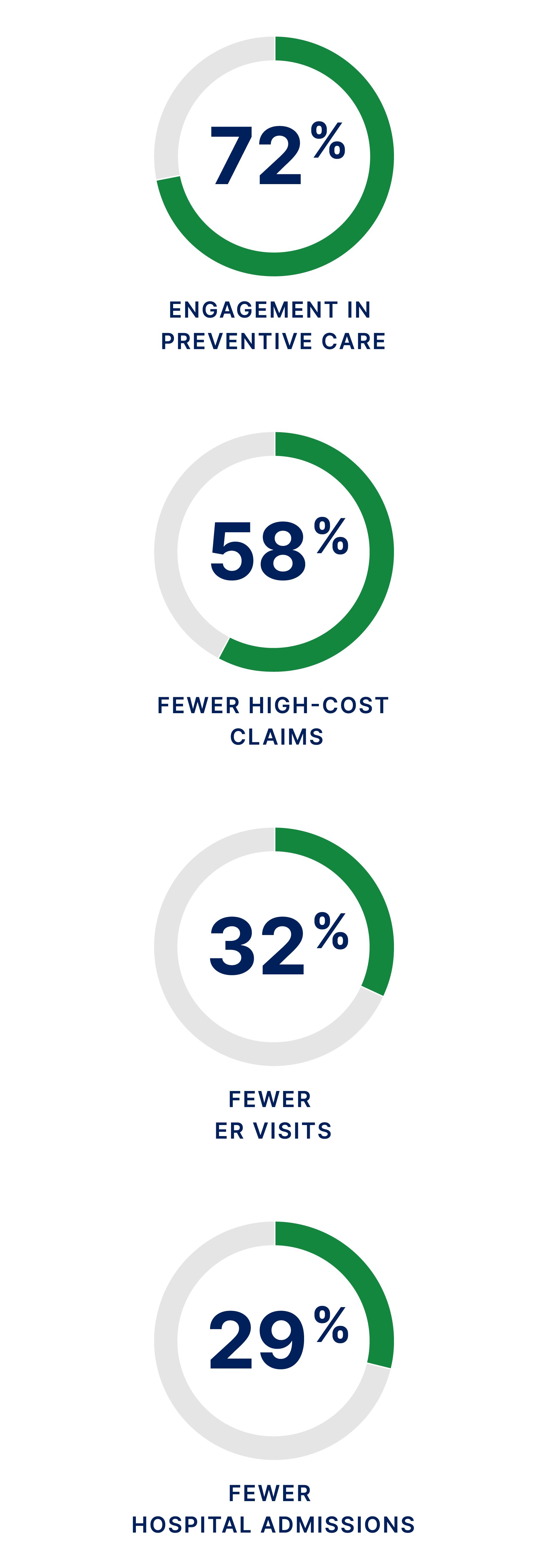
KelseyCare Delivers:
- 15-30% lower total medical cost
- top quality care, and
- high member satisfaction.
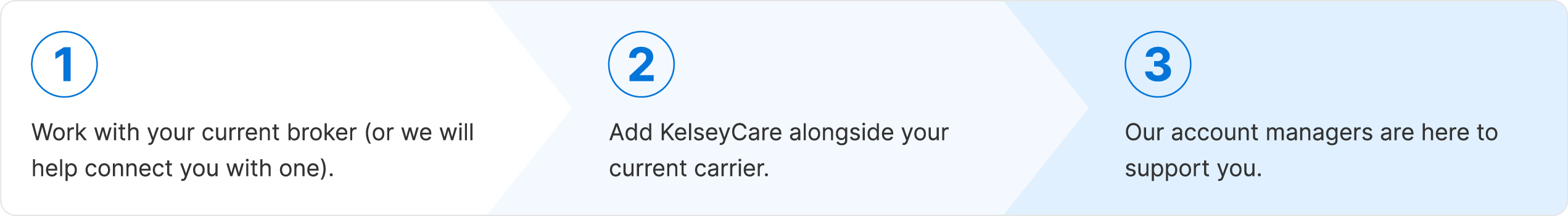
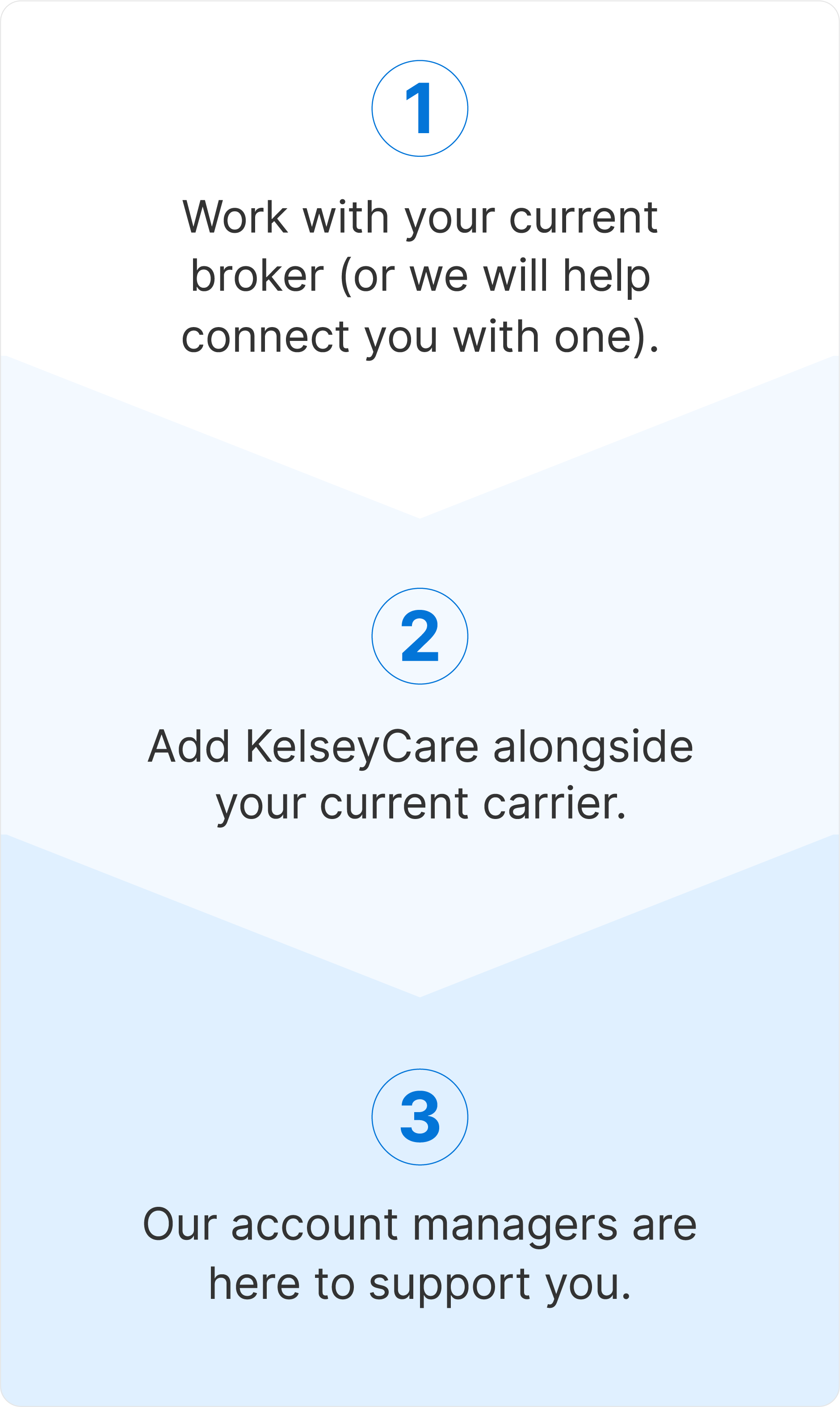
400+ Greater Houston companies including some of the city’s largest businesses, municipalities, and school districts rely on KelseyCare as a key part of their benefits strategy.

CEO of Barrios Technology, Sandy Johnson, experienced the value of coordinated care first-hand. Hear her story and how the exclusive KelseyCare programs save the employer and member money, while helping families live healthier lives.

Albert Mireles, from Hunton Group, discusses the value of KelseyCare Health Plans in managing both employee health and healthcare costs. Hear how KelseyCare's exclusive programs have made a positive impact for both the business and its employees, providing a sustainable solution for managing care and cost.
As the region’s only NCQA-accredited Accountable Care Organization (ACO), KelseyCare is fundamentally different from any other health plan with one goal in mind: improving health.
Healthier Employees. Healthier Bottom Line.